In Canada nearly 8 million individuals suffer from chronic pain, and 70% of those are women. We recognize that medical professionals often do not know how to manage complex chronic pain as it relates to gynecological/pelvic disorders and invisible illness because of the interactions pain has with the reproductive and endocrine systems. As our plan was to develop a pain management clinic for those assigned female at birth – creating a safe space for both cis-females and those who identify otherwise – we needed to make sure that the overarching goal of specialized, multi-disciplinary care in this area of health would make a difference on someone’s decision to try alternative therapies.
Method:
We conducted a survey that was open to the public that would answer the most pressing questions about our business model. We primarily used social media outlets and word of mouth to get a substantial representation of genders, geographies and illnesses.
Inclusion Criteria:
This survey was open to
· people assigned female at birth
· living in Canada and
· suffering from chronic pain.
A total of 179 participants from across Canada completed our survey.
Understanding what types of illnesses our responders suffer from was key to the open text questions we designed in the survey. We asked 1) what has helped with chronic pain, and 2) of the services we hope to provide, have any been helpful in reducing chronic pain.
30 of 54 (55%) patients with Pelvic Pain Disorders have tried and had success with Pelvic Floor Physiotherapy. For the remaining 24, there was a variety of answers ranging from ‘I haven’t tried’, ‘I can’t afford it’ and ‘It did not work’.
Those who deal with heightened pain receptors on the skin’s surface such as those with fibromyalgia and lupus often reported heat and rest to be the main aids for reducing chronic pain. Similarly, patients with ME/CFS and rheumatoid arthritis also mention heat as a source of reprieve, in addition to light massage or physiotherapy.
For those with IBS, responders either omitted any detail regarding IBS treatment (but listed out effective treatment for their other co-morbidities) or they mentioned changes in diet (low fodmap, restriction).
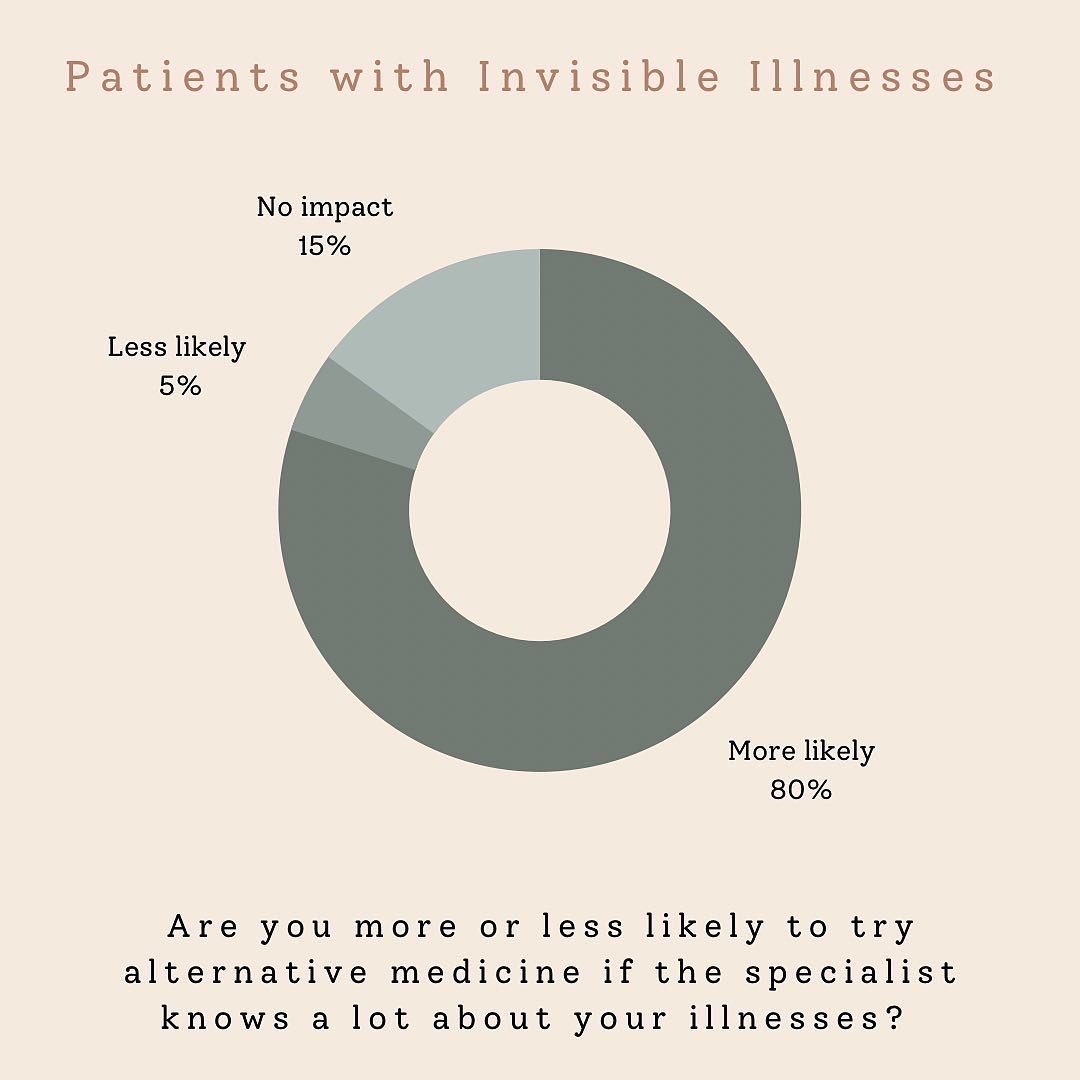
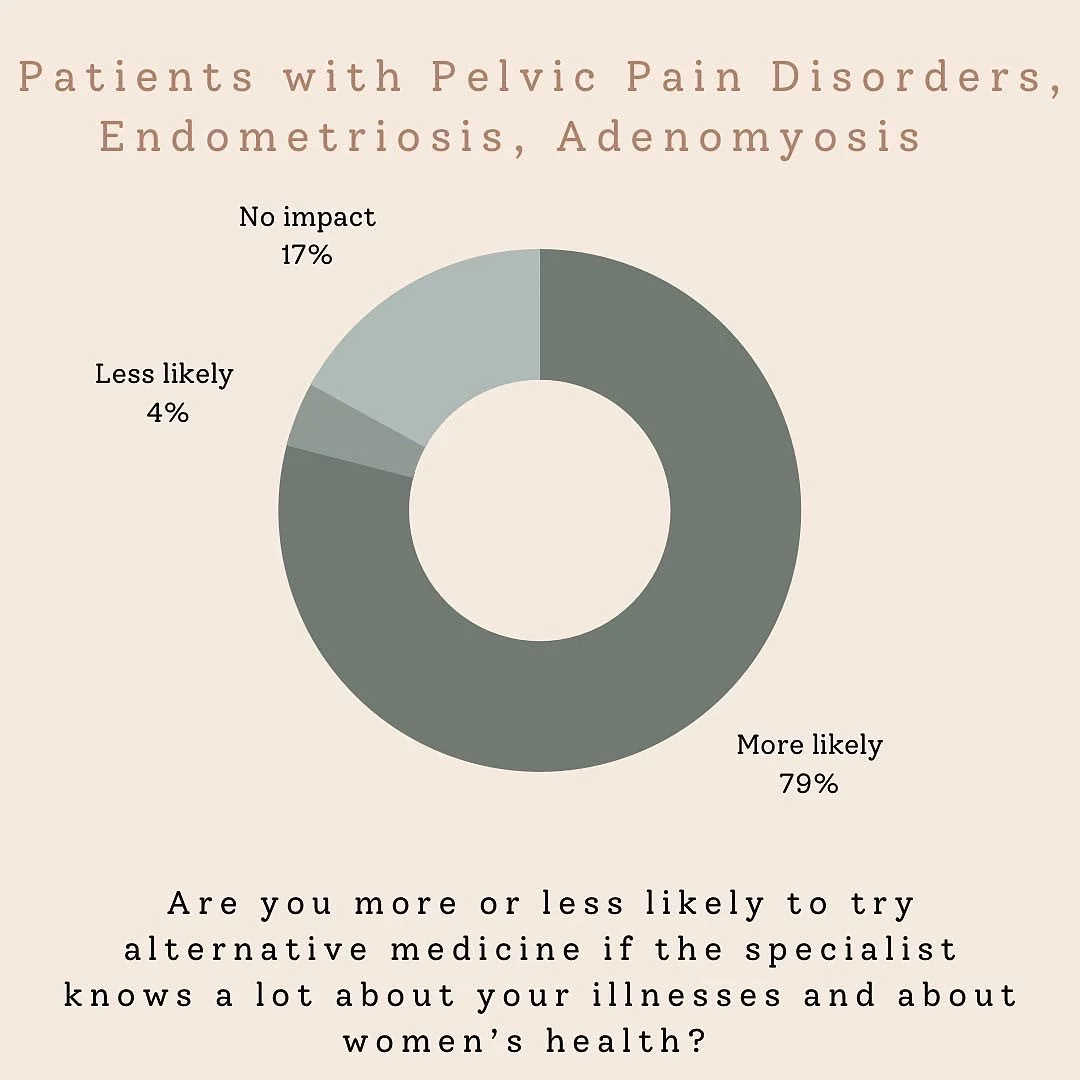
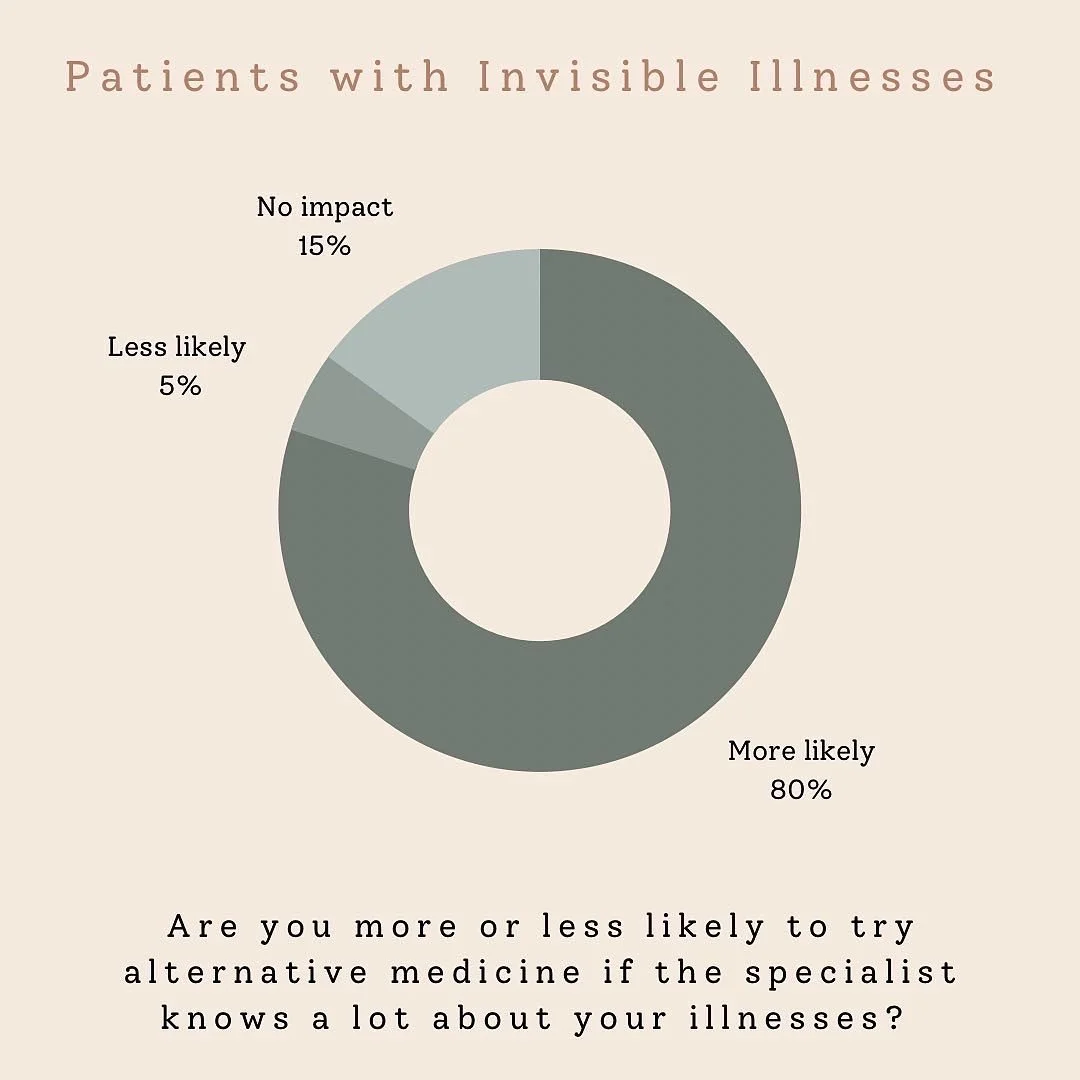
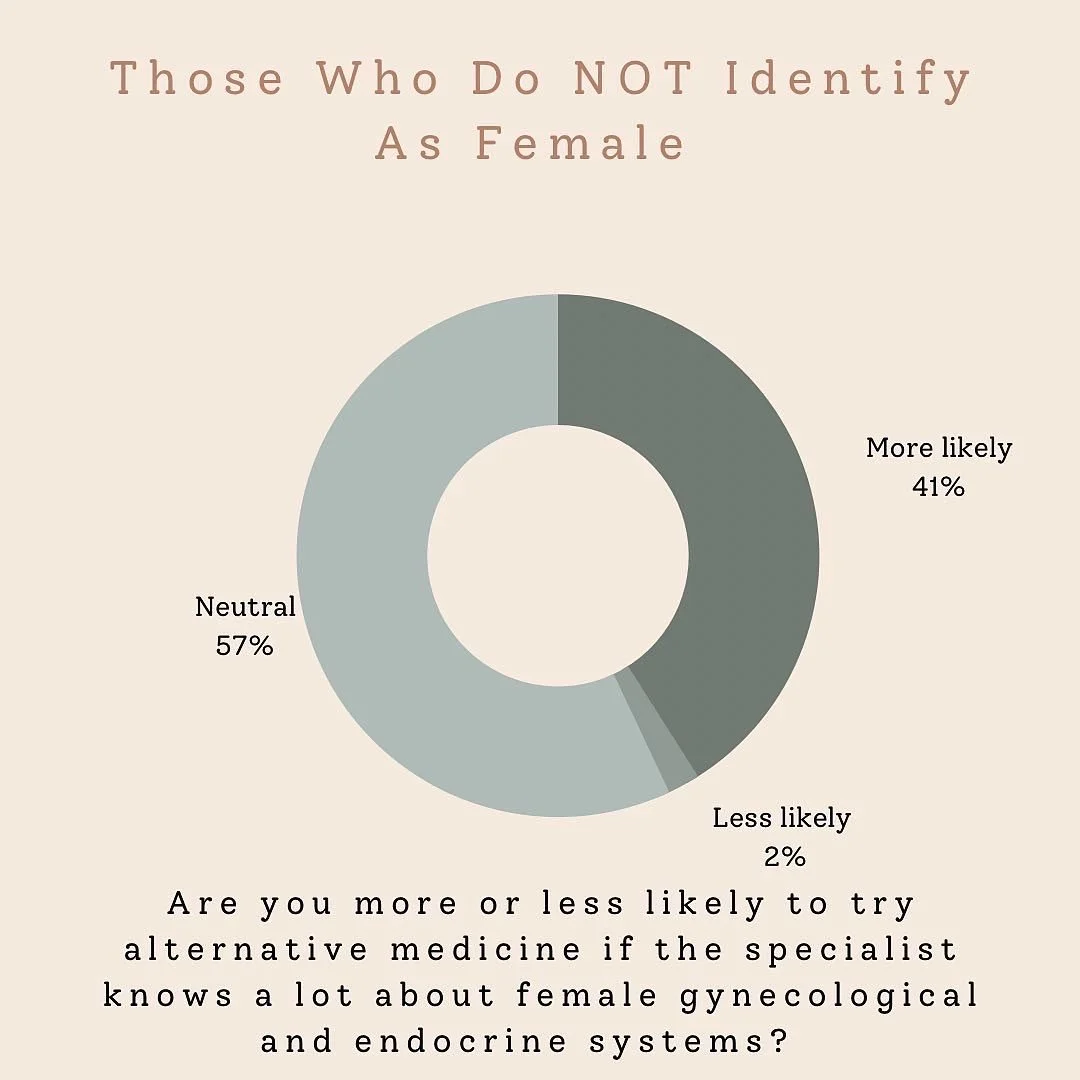
Subsequently we asked some poignant questions to better understand our goals for Femade.
The data speaks for itself.
Note that of those who responded neutral in the identity question, all identified as female.
Ordinarily a business would not rely on government subsidies or private healthcare to impact the success but with our model being immersed in the healthcare system we wanted to better understand peoples’ comfort levels in exploring these treatment options given the varying subsidies offered publicly and privately.
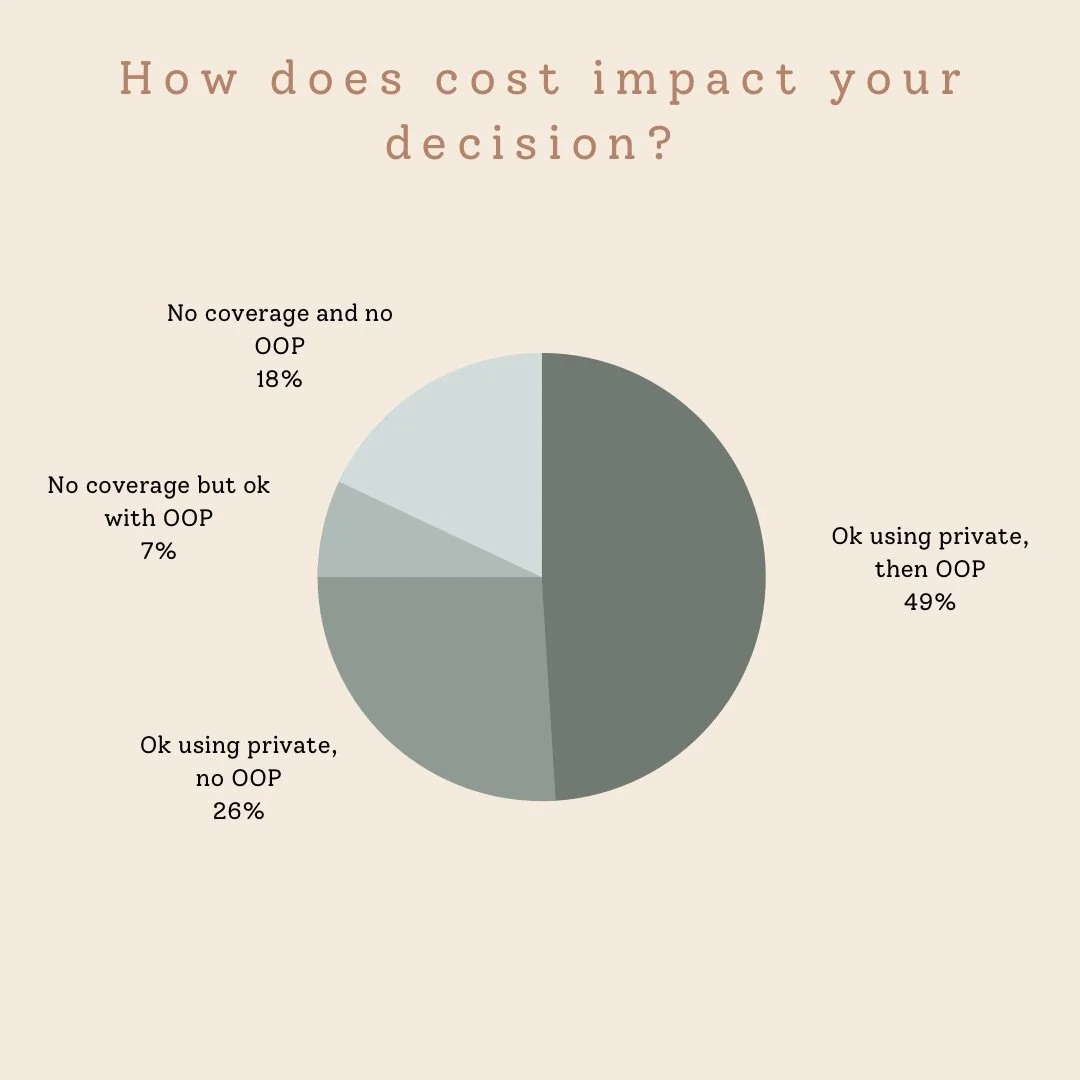
We asked: How does cost affect your decision to try alternative medicine?
Nearly 50% of our responders were willing to pay Out of Pocket after their private coverage elapsed. An additional 7% were comfortable merely paying out of pocket. That speaks volumes to how effective these treatment modalities have been and can be for patients suffering from chronic pain.