PELVIC PAIN
Definition
Pelvic pain is often associated with menstruation and presents with symptoms of heavy bleeding, painful menstruation (dysmenorrhea), cramping, fatigue and a host of secondary symptoms associated with the perpetual loss of blood. Under this banner, we look at primary dysmenorrhea, and causes of secondary dysmenorrhea. Separately, we talk about pain associated with the cervix, vagina and the vulva.
Pelvic pain in the medical system can get confusing as it can be categorized as gynecological, gastrointestinal, urological, neurological or musculoskeletal; this is a result of the complex mapping of systems within the pelvis nestled above the pelvic floor.
Thus in light of the complexity of pelvic pain and its mechanisms: Chronic Pelvic pain, by definition, is defined as non-cyclic, non-menstrual pelvic pain persisting >6 months, restricted to below the umbilical cord.
literature - Diagnosis and Treatment of pelvic pain
Many adolescents experiencing dysmenorrhea have primary dysmenorrhea which is painful menstruation in the absence of a pathology or stimulus. Research has shown that the menstrual blood of those with painful periods often express different levels of biomarkers that would increase cramping and pain associated with menses, namely prostaglandin PGF2a and leukotrienes which are both inflammatory mediators. The first line of defense for patients presenting with primary dysmenorrhea is the use of non-specific anti inflammatory drugs (NSAIDs) such as Advil, as it has shown to reduce inflammation and improve quality of life for these individuals. The inflammation can be monitored over time with the efficacy of these pain alleviators, however, depending on the severity and frequency of bleeding the patient may be put on hormonal therapy simply for cycle regulation.
About 10 percent of affected {persons} do not respond to these measures. It is important to consider secondary causes of dysmenorrhea in {persons} who do not respond to initial treatment. - Coco et al.
If a patient does not respond well to NSAIDS, it tends to point to secondary dysmenorrhea which is painful menstruation due to the presence of a stimulus/disease such as endometriosis and/or adenomyosis. At that point a patient should undergo further testing including imaging such as ultrasound, and should be referred to a specialist for medical management.
Other causes of pelvic pain, without the classic symptoms of endometriosis/adenomyosis are factors like fibroids, ovarian cysts, and polycystic ovarian syndrome (PCOS). Lastly, pelvic pain may be the result of any number of factors such as those mentioned above.
Not much research has been done to examine the efficacy of holistic approaches to pelvic pain. However, the findings do show compelling results when using acupuncture (with and without moxabustion) to reduce the pain and inflammation associated with pelvic pain. It has been show that acupuncture downregulates inflammatory cells and cytokines and thus may subsequently cause an analgesic affect.
Survey Results
what they told us
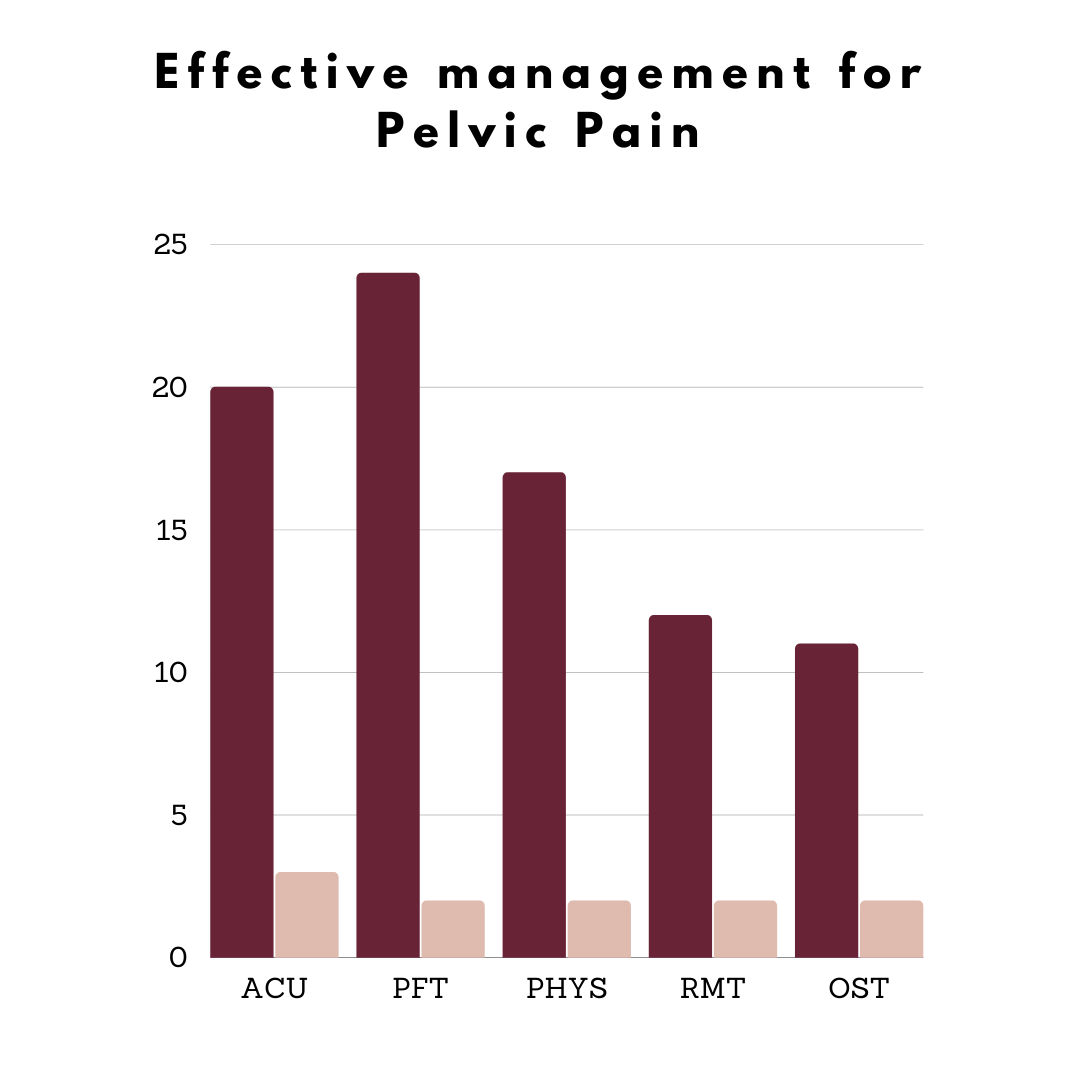
Without a doubt, pelvic pain is being managed by a wide range of manual services. For more information see our Survey Summary.
In the context of our survey we see that pelvic floor physiotherapy is being sought after in this population, which is absolutely what we would recommend. We were pleased to see that patients are seeking out acupuncture though it is much less spoken about with gynecologists and family doctors; the data is promising. While we did not sufficiently differentiate between pelvic floor physiotherapy and physiotherapy we suspect these patients are in fact utilizing pelvic floor physiotherapy. Furthermore, as the nuance between pelvic pain and chronic pelvic pain is not often used in the patient community we are not clear how many responders would classify themselves as having chronic pelvic pain vs cyclic menstrual pelvic pain.
Femade Approach to treating & Managing pelvic pain
Since the etiology of pelvic pain is not always understood at the onset of meeting a patient, it is critical that practitioners determine whether the origins and pathways of pain are considered more systemic (ie the organs themselves, the orientation of the pelvis, the surrounding hypertensive muscles), related to menstruation (ie primary or secondary dysmenorrhea), neuronal (ie the innervating nerves themselves) vs nociplastic (residual ‘central sensitization’ or heightened pain signals lasting after the stimulus as been removed).
When it comes to treating and managing pelvic pain, we always introduce pelvic floor physiotherapy and acupuncture to the patient. The pelvic floor physiotherapy gives us a better understanding of the range of motion, and areas of sensitivity within the pelvic area. We then try to layer the utility of the acupuncturist who - using a combination of intake methods - can help the body channel more resources to the affected area. Frankly, the needles can be placed in a variety of combinations to achieve results. Thirdly, if the patient is amenable we do like to add in massage therapy as pelvic pain - either cyclic or chronic - can take a toll on the muscles throughout the body. This not only impacts the soreness of the muscles but can affect sleep and mood.
Depending on the nature of the pelvic pain it may be of great benefit to incorporate naturopathic medicine. In some cases it can help with adjusting hormones, supplementing resources that the body is lacking, and identifying triggers such as food and lifestyle.
Lastly, pelvic pain is grossly misunderstood! We offer psychotherapy to address some of the root causes of stress, and stress management. We also offer peer support for a more casual mental health support outlet as well as virtual group support sessions to help build a community.
Resources
New developments in the pharmacotherapy of neuropathic chronic pelvic pain https://pubmed.ncbi.nlm.nih.gov/28116131/
Acupuncture for Primary Dysmenorrhea: A Potential Mechanism from an Anti-Inflammatory Perspective https://pubmed.ncbi.nlm.nih.gov/34899943/
ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent https://pubmed.ncbi.nlm.nih.gov/30461694/
Primary dysmenorrhea https://pubmed.ncbi.nlm.nih.gov/10465224/