RHEUMATOID ARTHRITIS
Definition
Rheumatoid Arthritis (RA) is a chronic autoimmune disease in which there is progressive and symmetrical inflammation in the joints, resulting in cartilage destruction, bone erosion and disability. While there are many types of arthritis, rheumatoid arthritis being an autoimmune subtype means the body’s own immune system is attacking itself. There is great importance in diagnosing and treating this disease as quickly as possible simply because of how it manifests if untreated.
It is suggested that 0.4%-1.3% of the population is affected by RA, with almost twice as many women than men, and greater incidence after the age of 60. Patients may complain of a few joints being impacted early on, with more joints being affected as the disease progresses.
LITERATURE - DIAGNOSIS AND TREATMENT OF rheumatoid arthritis
Some of the earlier signs of RA are fatigue, flu-like feeling, swollen and tender joints, and morning stiffness. If left untreated these symptoms can evolve to pleural effusions, lung nodules and many other symptoms.
Diagnosis often involves - like many of the invisible illness - the patient’s commentary on symptoms and severity. Quality of life is a big marker for onset of RA. An ultrasound can be done on the joints to snapshot to see any signs of inflammation or eroding. Blood markers such as C-reactive protein - a general inflammatory marker - and ESR can be tested, along with RA-specific antibodies in the blood.
The goal of early treatment is to put the patient into remission entirely or to at least decrease the severity of symptoms within a 6 month timeframe. Treatment then follows a ladder approach, starting with bed rest to reduce the inflammation, along with trial of non-specific anti-inflammatory drugs such as ibuprofen. The next approach is a trial with disease-modifying anti-rheumatic drugs. In addition to this pharmacology trial, patients are recommended to begin routine physiotherapy to help move the joints and reduce inflammation. Next, patients can try methotrexate which often results in decreases symptoms and increased quality of life. A limited number of patients may not respond to this medication and can be put on biologics specific to RA.
…it is difficult for patients to tolerate {drug therapy} due to the long period of traditional drug therapy and large adverse reactions. Therefore RA patients still need complimentary and alternative therapies to seek additional remission or therapies with fewer side effects. ~Shang et al.
As described above, physiotherapy has been a widely accepted treatment therapy for those with RA. Similarly, patients can have gentle pressure applied to their joints to help loosen the ‘stiffness’. In both of these approaches the patient is introduced to subtle but increasing movements as to increase movement but not increase pain. Additionally, acupuncture has been shown to decrease the progression of the disease, alleviate the pain, and improve joint function.
Survey Results
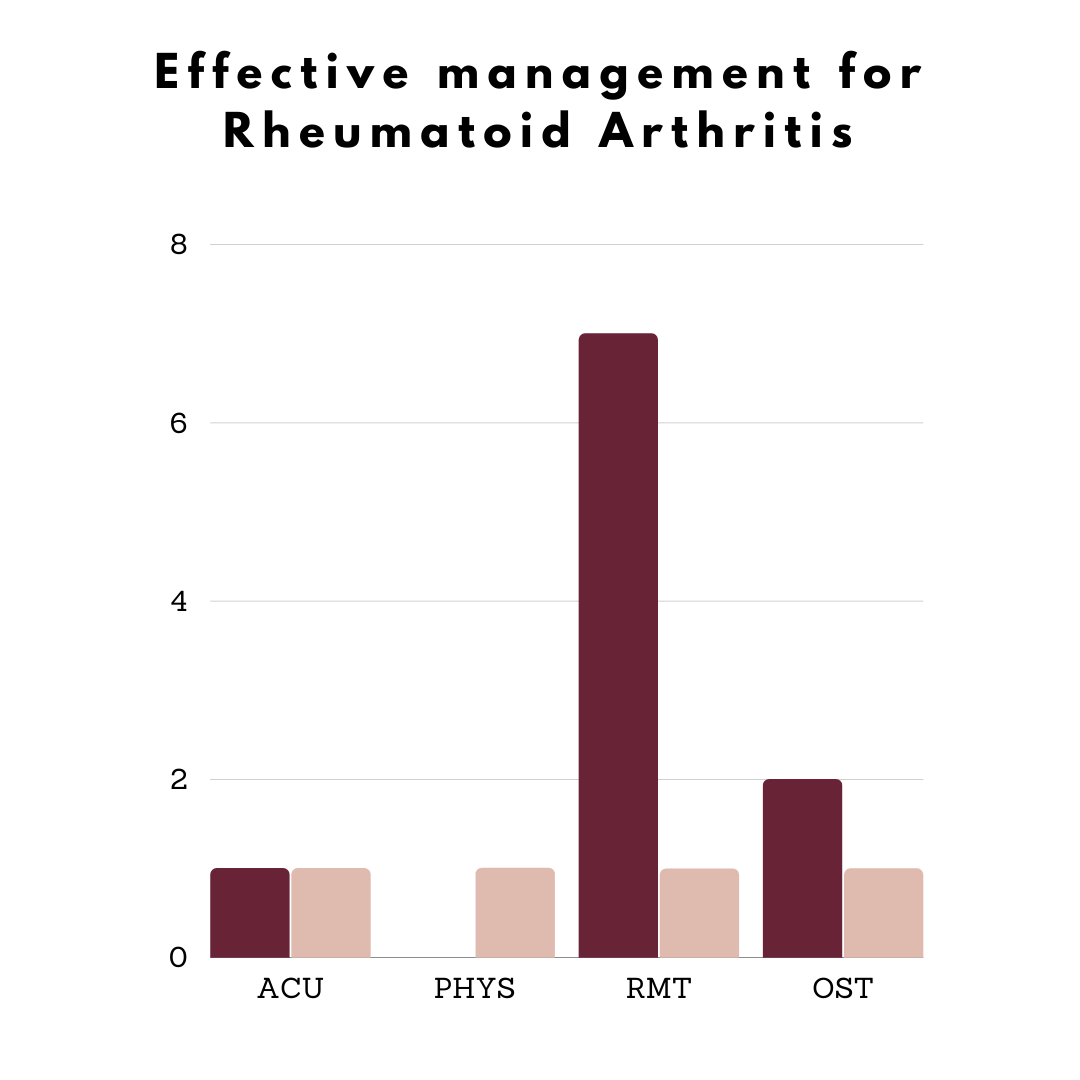
Unfortunately our national survey was not able to capture a large number of individuals suffering from RA. The evidence does point to the utility of massage therapy which makes sense both from a physical and mental reprieve of pain. It is somewhat shocking to see the patients are not utilizing physiotherapy which is often recommended by rheumatologists but rarely covered by provincial healthcare.
what they told us
While the data is lacking, we can see a trend towards Registered Massage Therapy for the management of Rheumatoid Arthritis. For more information see our Survey Summary.
FEMADE APPROACH TO TREATING rheumatoid arthritis
Using physiotherapy to address which joints are affected and the range of motion in these joints, we can then introduce safe moments to gradually increase motility while decreasing pain. The physiotherapy approach is widely accepted in the medical system and is often included in inpatient treatment, as well as recommended outpatient management. Here at Femade we truly do believe in safe movement and that means moving at a pace that improves quality of life, and slow the progression of RA. Similarly, with massage therapy, light and increasing pressure can be applied with the same approach of reducing inflammation, increasing safe movement and addressing the pain.
Acupuncture is becoming widely accepted for RA management. Treatment is not only aimed at the particular joints that are inflamed and causing pain, but also looks at gut health which is a root origin for many autoimmune diseases. Understanding the patient’s RA symptoms as well as other comorbid symptoms helps to address the root causes and create a plan with the patient to improve quality of life.
Nutrition and lifestyle are also key features in slowing the progression of this disease. For Naturopathic Medicine the key is to look at lifestyle cues that tell us what areas we need to focus on. We can address the inflammation, any immune factors that could be exacerbating symptoms, and we can address underlying symptoms such as restless sleep. Nutrition builds on this concept to investigate trigger foods that often increase inflammation, and then to build a plan around meals that are nutritious and safe.
Lastly, understanding that RA is largely frustrating and misunderstood, we offer psychotherapy to address some of the root causes of stress, and stress management. We also offer peer support for a more casual mental health support outlet as well as virtual group support sessions to help build a community.
Resources
Update on the Pathomechanism, Diagnosis, and Treatment Options for Rheumatoid Arthritis. https://pubmed.ncbi.nlm.nih.gov/32260219/
The efficacy and safety of acupuncture-related therapy in the treatment of rheumatoid arthritis. https://pubmed.ncbi.nlm.nih.gov/34397895/