In March - Endometriosis Awareness Month - we sat down with Michelle M - or otherwise known on social media as The Happy Pelvis. Michelle has been actively educating others about Pelvic Floor Dysfunctions at large. We sat down virtually to learn more about Michelle’s story, not only with Endometriosis and Pelvic Pain but about her battle with Fibromyalgia and Lupus.
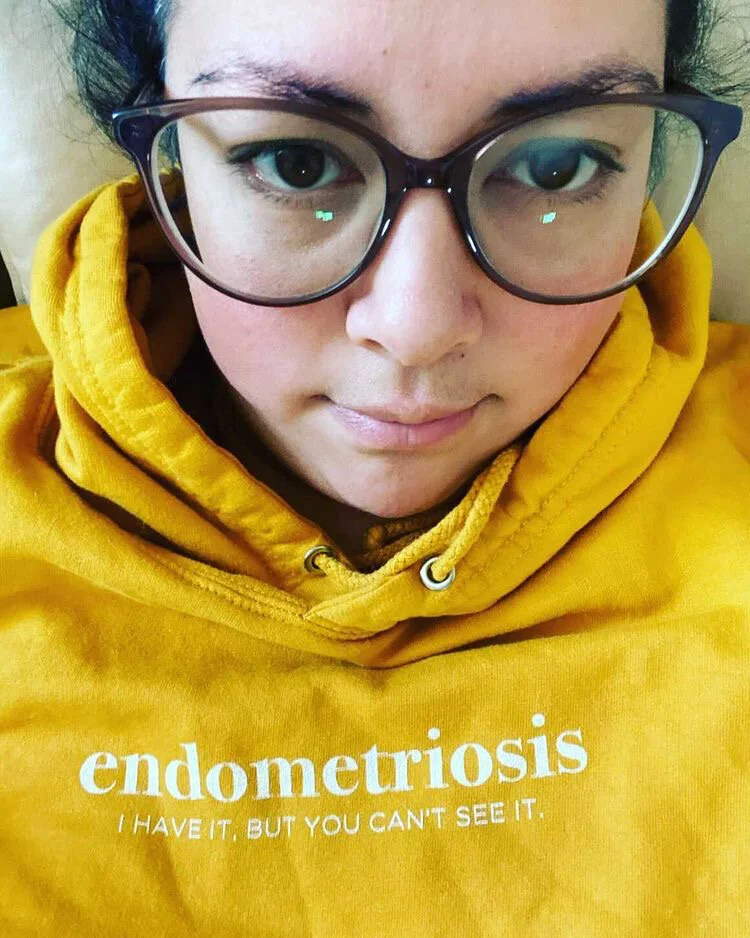
I’m Michelle M. and I am a 31-year-old pelvic health advocate that lives in Mississauga, a city just outside of Toronto, Canada. I am also the creator of The Happy Pelvis: an online blog and platform that aims to educate and spread pelvic health awareness in Canada and around the world. But my main role is a full-time chronic pain patient, who is trying to find relief and ultimately, a better quality of life.
In 2018, I had to temporarily leave my graphic design position at one of Canada’s top media companies due to the start of debilitating painful flare ups that I still suffer from today.
At 28 years old, after over 15 years of searching for answers, I received the diagnosis of Pelvic Floor Dysfunction, IC/Bladder Pain Syndrome, Endometriosis, Fibromyalgia and Lupus.
“Our muscles aren’t meant to be tight all the time and after a while, they start to develop trigger points in these muscles. These trigger points then cause pain. ”
The pelvic area resides so closely with other organs, and many of the issues you experience are all so close together in proximity. Can you describe what your pain feels like? If possible, can you tie the pain to the disease?
When it is at its worst, it is a debilitating flare up that feels like a UTI on steroids with a side of razor blades and intense cramping. With pelvic pain, it can be quite difficult to narrow down pain generators but below are some of my painful symptoms related to each condition I have been diagnosed with.
Endometriosis: Debilitating cramping throughout week of period, heavy flow with large clots, sharp/shooting pain with bowel movements/digestion, painful penetration, sciatic pain
Interstitial Cystitis/Bladder Pain Syndrome: Ache with pain in lower abdomen and burning/stinging with urination that can feel like peeing razor blades, constant urinary frequency and retention which leads to more burning.
Vulvodynia driven by hypertonic Pelvic Floor Dysfunction: A whole lot of different pains and sensations that ebb and flow throughout the day. But overall burning/stinging, itching, tearing pain on vulva, vestibule, urethra and vaginal opening. Triggered by touch, sitting, movement, and even standing.
Pelvic Floor Dysfunction: Burning with urination, painful penetration (which persists days to weeks after: ache and feeling like I have been beaten up from the insides), sharp hip pain with lack of mobility, and tailbone shooting pain and ache… just to name a few.
Fibromyalgia + Lupus: pain, stiffness, swelling, tenderness/heat in joints, painful mouth sores.
Since you do have a few different illnesses that you are working with, how did the progression of diagnosis go for all of these?
Sadly, it has been a long journey. I have lived with pelvic pain chronically since childhood, after a tobogganing incident where I injured my tailbone on an icy hill. I never fully recovered and my tailbone has always been a sore spot that I began to guard unwillingly, but adapted and learned to live with. I then moved into puberty with extremely painful and heavy periods, chronic urinary tract infections, yeast infections; which snowballed into getting on birth control and being diagnosed with Vulvodynia, Vestibulodynia, and possible Lichen Sclerosus by a Gynaecologist. All by 16 years old.
In my early 20’s, after years of continuous pain and antibiotic use, I unfortunately suffered a severe reaction to my Achilles tendons from a urinary tract infection antibiotic, Ciprofloxacin.
From that point, I began to search elsewhere, other than western/modern medicine for answers. I saw a Naturopath and she threw the word Interstitial Cystitis at me based on my symptoms and treated my recurrent UTI’s and bladder as if I had IC and my issues slightly improved. In late 2017, at 28, I treated a UTI but my symptoms never went away. All of my tests and scans were not showing anything or came back inconclusive. In 2018, after advocating for myself, I was officially diagnosed with Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS), Endometriosis, Pelvic Floor Dysfunction (PFD), as well as Fibromyalgia and Lupus.
Did any of your doctors tell you that you have X because it’s more prevalent in women with Y? Just wondering if there is a clinical link between anything you’re battling.
After finally getting in to see the right pelvic pain specialist in 2018, and getting my PFD and IC/BPS diagnoses, I was told that Endometriosis was prevalently seen in patients with Interstitial Cystitis and Pelvic Floor Dysfunction I was then told that surgery for endometriosis was needed to confirm diagnosis. They were right; Endometriosis was found.
Endometriosis is sometimes known as the “Evil Twin” to IC/BPS, yet they are two separate conditions and inflammatory processes. Endometriosis needs to be treated by excision of the Endometriosis tissue and IC/BPS is managed through medical pain management and lifestyle changes.
What are some of the more modern medicine techniques that have worked for you?
I wish I could tell you that I have found something that has worked for me, but I am still on my journey to find it.
Right now, it is a combination of things like compound suppositories, pain medication and pelvic floor physical therapy that are helping me manage my pain.
Compound Suppositories:
1. Amitriptyline (Nerve medication), Gabapentin (Nerve medication), Diazepam (to relieve muscle spasms)
2. Baclofen (Muscle Relaxant), Diazepam (to relieve muscle spasms) and Ketamine (Pain medication)
Pelvic Floor Physical Therapy 2x per week.
Have you ever reached a point where you had to think outside the modern medicine box? If so, what did you do that helped with the pain?
In 2014, I had a severe reaction to an antibiotic and was unable to walk due to the effect it had on my Achilles tendons. At that point, I wanted to step away from western medicine because all it had done was made me worse. I ended up making an appointment to see a Naturopath who then helped me get my bladder pain and chronic UTI’s better controlled using alternative therapies.
My family doctor referred me to a Pelvic Pain Program at a local University where I educated myself on the science of chronic pain and techniques to cope such as mindfulness and pelvic floor stretches.
Generally speaking, are you open to alternative therapies such as osteopathic, pelvic floor, myofascial massage, acupuncture?
Yes, I definitely am open to alternative therapies.
It’s funny you mention Pelvic floor PT and Myofascial massage because those are such an important component in the treatment of chronic pelvic pain. This is because our muscles tighten and tense up when they are injured or when we are in pain. This is a normal response in our bodies to prevent more damage from occurring. Our pelvic floor muscles tighten up too when there is something painful in the pelvis. This is why we need Pelvic Floor Physical Therapy. Our muscles aren’t meant to be tight all the time and after a while, they start to develop trigger points in these muscles. These trigger points then cause pain. Trigger points, muscle tightness, and inflammation can irritate the crazy amount of nerves in the pelvis, which can cause pain to continue throughout the pelvis and surrounding areas.
I also swear by Pelvic Floor Therapy. What would you tell our readers in order to help them consider alternative therapies?
By taking the leap and giving alternative therapies a try, you are taking your health into your own hands.
I learned the most about my body through the alternative care practitioners I’ve met along the way and I am forever grateful.
And lastly, what would you tell your younger self about pain management?
Speak up. Tell them you are in pain and it’s all that you can think about.
I didn’t talk about my pelvic pain enough due to the stigma and embarrassment that came along with it at such a young age. Once my doctors told me there wasn’t anything else they could do for me and it was something I had to live with, I began to keep my pelvic pain hidden away from everyone around me and smiled through the suffering.
I wish I spoke up and insisted on better care and further medical exploration.
Anything else you want to tell our readers?
If you live with pelvic pain, be gentle with yourself, you are not alone.
There is hope, there is help and you can get better.
~ Michelle
The Ultimate Vulvodynia and Pelvis Pain Resource Guide